Having Lower Back Pain? Here’s Why You Should Delay Your MRI
Reference
Shraim, B., Shraim, M., Ibrahim, A., Elgamal, M., Al-Omari, B., & Shraim, M. (2021). The association between early MRI and length of disability in acute lower back pain: a systematic review and narrative synthesis. BMC Musculoskeletal Disorders, 22(1). https://doi.org/10.1186/s12891-021-04863-9
Objective
There is speculation that healthcare professionals may over-interpret the structural defects seen on MRI and prescribe invasive interventions, despite countless evidence showing that severity of MRI findings do not always correlate with intensity of symptoms. Patients who attempt to self-interpret the scan results may also be misled, leading to unnecessary worry and distress.
This study aims to examine if getting an early MRI (eMRI) leads to prolonged Length Of Disability (LOD) in patients with acute lower back pain (LBP).
What they did
What they found
Difference in days of LOD:
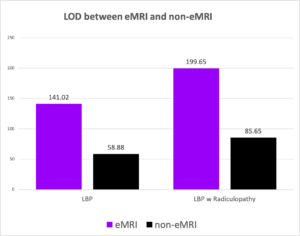
- On average, LBP patients in the eMRI group had 82.14 more days of LOD compared to the non-eMRI group (1 year of follow up)
- On average, LBP patients with radiculopathy in eMRI group had 114 more days of LOD compared to the non-eMRI group.
Difference in Hazard Ratio:
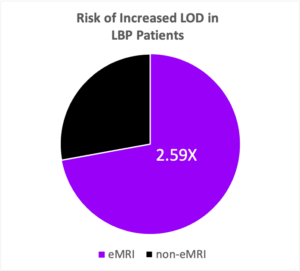
- On average, LBP patients in the eMRI group is 2.59 times more likely to experience increased LOD compared to the non-eMRI group.
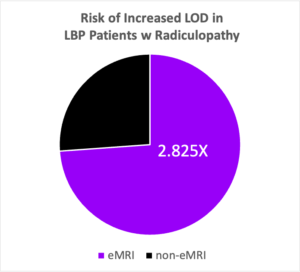
- On average, LBP patients with radiculopathy in the eMRI is 2.825 times more likely to experience increased LOD compared to the non-eMRI group.
Limitations
- Number of studies was relatively small, with only 7 studies from 5 populations in the US. Generalisability is limited to the US population.
- LOD was measured using number of days of wage replacement. The strength of association may be underestimated as termination of wage replacement does not imply full recovery or work resumption.
- Using days of wage lost as measurement meant that other predictors of LOD were overlooked, such as level of functional disability, work accommodation, nature of job, fear-avoidance, and other comorbidities including psychiatric conditions.
- Meta-analysis was not possible due to between-study heterogeneity, which prevented result pooling.
Conclusion
eMRI is associated with increased LOD in patients with acute LBP.
Practical Takeaways
Here is one of the moments where ignorance is bliss. It is difficult to shake off the intuition that pain is associated with structural damage, but we now know from pain science that pain is a complex experience that can be modulated by numerous factors, such as stress, sleep quality and perceived social support. Rather than reflexively recommending imaging scans, healthcare professionals can be more prudent by considering other psychosocial factors that could have played a role in the patient/client’s pain experience.
We should also be wary of the language that we use to describe their condition, given that words can have a huge impact on how our patients/clients perceive their own state of health. The last thing we want is for them to develop a fear of movement and sink into sedentarism.